Abstract
Introduction
Cord blood transplantation (CBT) is increasingly being used as an alternative transplant method for patients without human leukocyte antigen-compatible related or unrelated donors. However, the outcome for some patients is poor due to a high relapse rate or non-relapse mortality (NRM). Pre-transplant assessment is important, especially in older patients or those with medical comorbidities.
An increase in intramuscular adipose tissue (IMAT) is associated with skeletal muscle (SM) weakness. Recent studies showed that the quality of SM can be evaluated by measuring IMAT content (IMAC) using computed tomography (CT) and that IMAC was also an independent risk factor for survival in patients following liver transplantation. IMAC was calculated by dividing the mean CT value for the multifidus muscle by the mean CT value for the subcutaneous fat (both in Hounsfield units). Using this method, we investigated the association between the quality of SM evaluated by pre-transplant IMAC and the transplant outcomes.
Patients and Methods
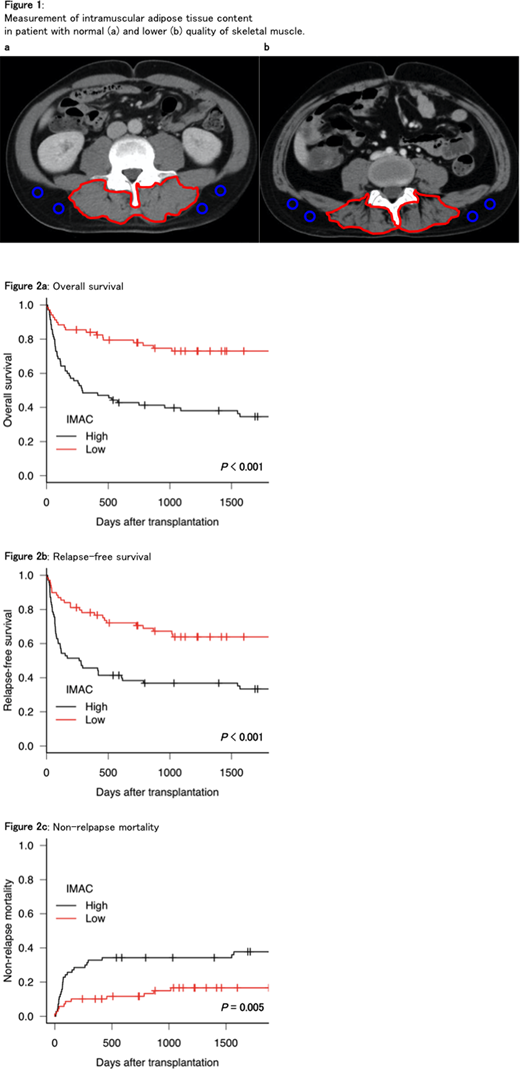
We included 139 patients who underwent their first single-unit CBT at our institution between January 2002 and December 2017. Pre-transplant CT was performed within one month before conditioning. The mean CT values for the multifidus muscle and subcutaneous fat were measured at the umbilical level by cross-sectional imaging. Subfascial muscular tissue in the multifidus muscle was precisely traced (Figure 1, red line). The CT values for the subcutaneous fat were measured at four regions of interest (Figure 1, blue circle) and the mean value was used. In general, IMAC is shown with a negative value, with a higher IMAC indicating a lower quality of SM. Patients were classified into the low IMAC group (male, < -0.43; female, < -0.29) and the high IMAC group (male, >= -0.43; female, >= -0.29) by the IMAC cut-off value based on the receiver operating characteristic curve.
We evaluated transplant outcomes such as overall survival (OS), relapse-free survival (RFS), NRM, and cumulative incidence of relapse (CIR) between the two groups. OS and RFS were estimated using the Kaplan-Meiyer test. NRM and CIR were calculated using Gray's method. Factors found to be significant (p < 0.1) through univariate analysis were further subjected to multivariate analysis, which was performed using the Cox proportional hazards regression model for OS and RFS and the Fine-Gray proportional hazard regression model for NRM and CIR.
Results
Among the 139 patients, 68 (48.9 %) were in the low IMAC group and 71 (51.1 %) were in the high IMAC group. The median age was 46 (range, 17 - 70) years. The underlying diseases were acute myeloid leukemia (n = 61), malignant lymphoma (n = 34), acute lymphoblastic leukemia (n = 23), myelodysplastic syndrome (n = 13), adult T-cell leukemia/lymphoma (n = 5), and others (n = 3). We found no significant differences between the two groups in terms of clinical characteristics including age, gender, performance status, underlying disease, hematopoietic cell transplantation-specific comorbidity index, disease status at CBT, or conditioning regimen.
The median follow-up period for survivors was 2,538 (range, 242 - 5,492) days. In total, 61 patients (43.9 %) died within three years after CBT: 26 (42.6 %) died of a relapse or progression of disease and 35 (57.4 %) died of non-relapse death. We observed a significant difference in OS, RFS and NRM between the high IMAC and low IMAC groups (high IMAC group vs. low IMAC group: three-year OS, 38.0 % vs. 73.0 %, p < 0.001; three-year RFS, 36.8 % vs. 63.9 %, p < 0.001; three-year NRM, 34.3 % vs. 16.6 %, p = 0.005; Figure 2). Multivariate analysis revealed that high IMAC was an independent adverse factor for OS (HR [95 % CI]; 2.95 [1.74 - 5.00], p < 0.001), RFS (HR [95 % CI]; 2.37 [1.45 - 3.87], p < 0.001), and NRM (HR [95 % CI]; 2.31 [1.14 - 4.72], p=0.020). Furthermore, in patients who received reduced-intensity conditioning (RIC) (n=75), high IMAC was an independent adverse factor for OS (HR [95 % CI]; 4.03 [1.73 - 9.35], p = 0.001) and RFS (HR [95 % CI]; 3.61 [1.69 - 7.73], p = 0.001).
Conclusion
To our knowledge, this is the first analysis that considers the prognostic impact of the quality of SM on the outcome of CBT. Our results indicate that increased IMAT is associated with a poor prognosis, especially in patients who received RIC. IMAC is a simple and objective measurement for evaluating the quality of SM and can be useful tool for predicting the outcome of CBT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal